Welcome to the 10TH Edition of The Clinical Chronicle!
As 2025 comes to a close, this edition reflects how rapidly medicine has evolved over the past year. Diseases once approached late, with few effective options, are now met with earlier diagnosis, targeted therapies, and precision strategies that are reshaping survival and quality of life.
This 10th Edition brings together 10 of the most practice-changing advances of 2025. These include blood-based diagnostics and durable disease-modifying therapy in Alzheimer’s disease, age-dependent cardiovascular protection with GLP-1 and SGLT2 therapies, and compelling evidence supporting broader use of SGLT2 inhibitors across the full spectrum of chronic kidney disease. We also examine CDC-endorsed twice-yearly injectable HIV prevention, the emergence of phenotype-driven biologics in COPD, and long-awaited survival gains in small cell lung cancer that are redefining frontline and relapsed care.
Together, these updates capture a year when treatment moved earlier in the disease course, became more precise, and began altering trajectories rather than reacting to advanced illness. This tenth edition closes a year where evidence truly changed clinical practice.
Stay sharp. Stay ahead.
Alzheimer’s Disease Enters the Era of Blood-Based Diagnosis and Durable Disease Modification
What Actually Changed in Alzheimer’s Care
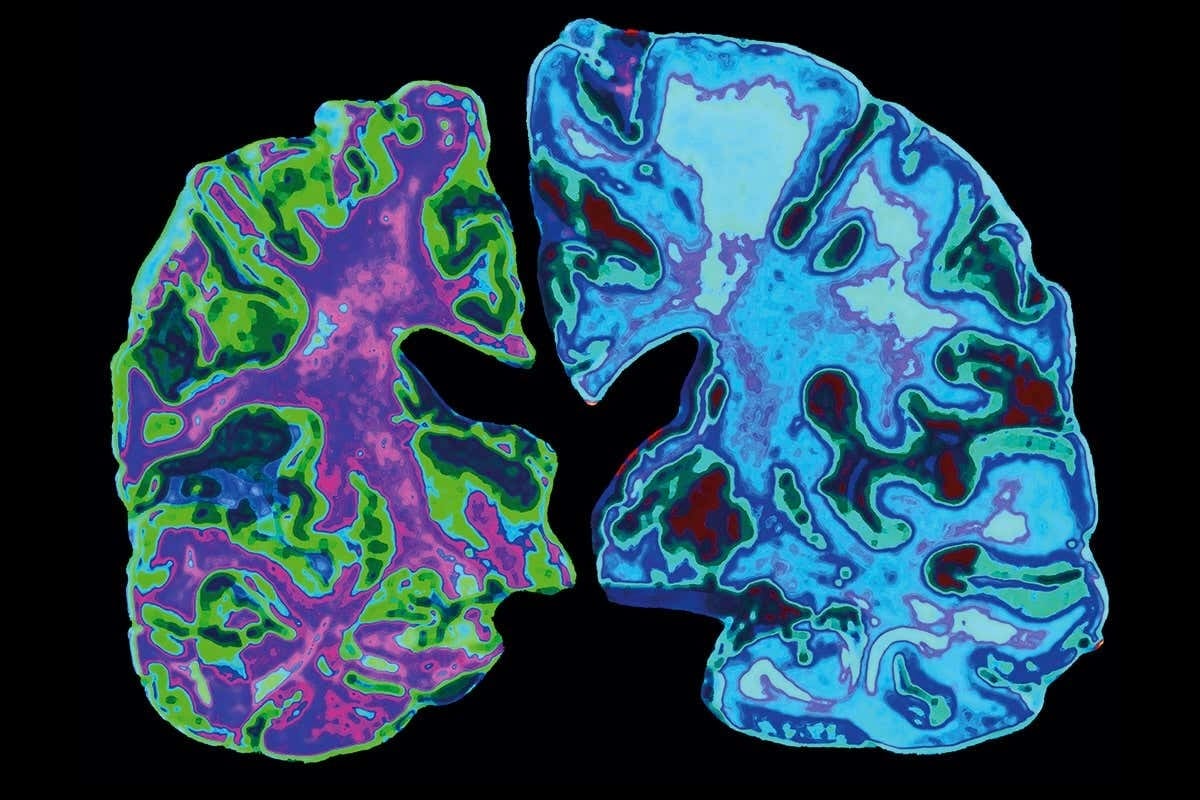
In a year when Alzheimer’s prevalence surpassed 7 million Americans, 2025 shifted the disease from late diagnosis and limited options to one where earlier detection, durable treatment benefit, and safer long term management became realistic in everyday practice.
Blood based diagnosis entered clinical care. The FDA approved the Lumipulse G pTau217 to β-amyloid 1–42 plasma ratio for symptomatic patients aged 55 and older and cleared the Elecsys pTau181 test for primary care. The Alzheimer’s Association endorsed blood biomarkers, allowing triage with 90% sensitivity and 75% specificity and definitive diagnosis without imaging when sensitivity and specificity reached 90%.
Long term treatment data strengthened confidence in disease modification. Lecanemab delayed progression to the next disease stage by about 30% with sustained benefit through 36 months, while donanemab reduced CDR-SB decline by 1.2 points at 36 months and lowered progression risk by 27% when started early. Functional modeling showed preservation of instrumental activities of daily living for 10 to 13 months in early disease.
Safety became more precise. The FDA mandated earlier MRI monitoring for lecanemab after identifying peak ARIA-E risk between the third and fifth infusions. A revised donanemab titration cut ARIA-E rates from 23.7% to 13.7% by week 24, and a subcutaneous lecanemab autoinjector improved real world feasibility.
Source: EISAI
Gene Editing Enters Clinical Reality
A one time CRISPR therapy achieves durable disease modification in hereditary transthyretin amyloidosis
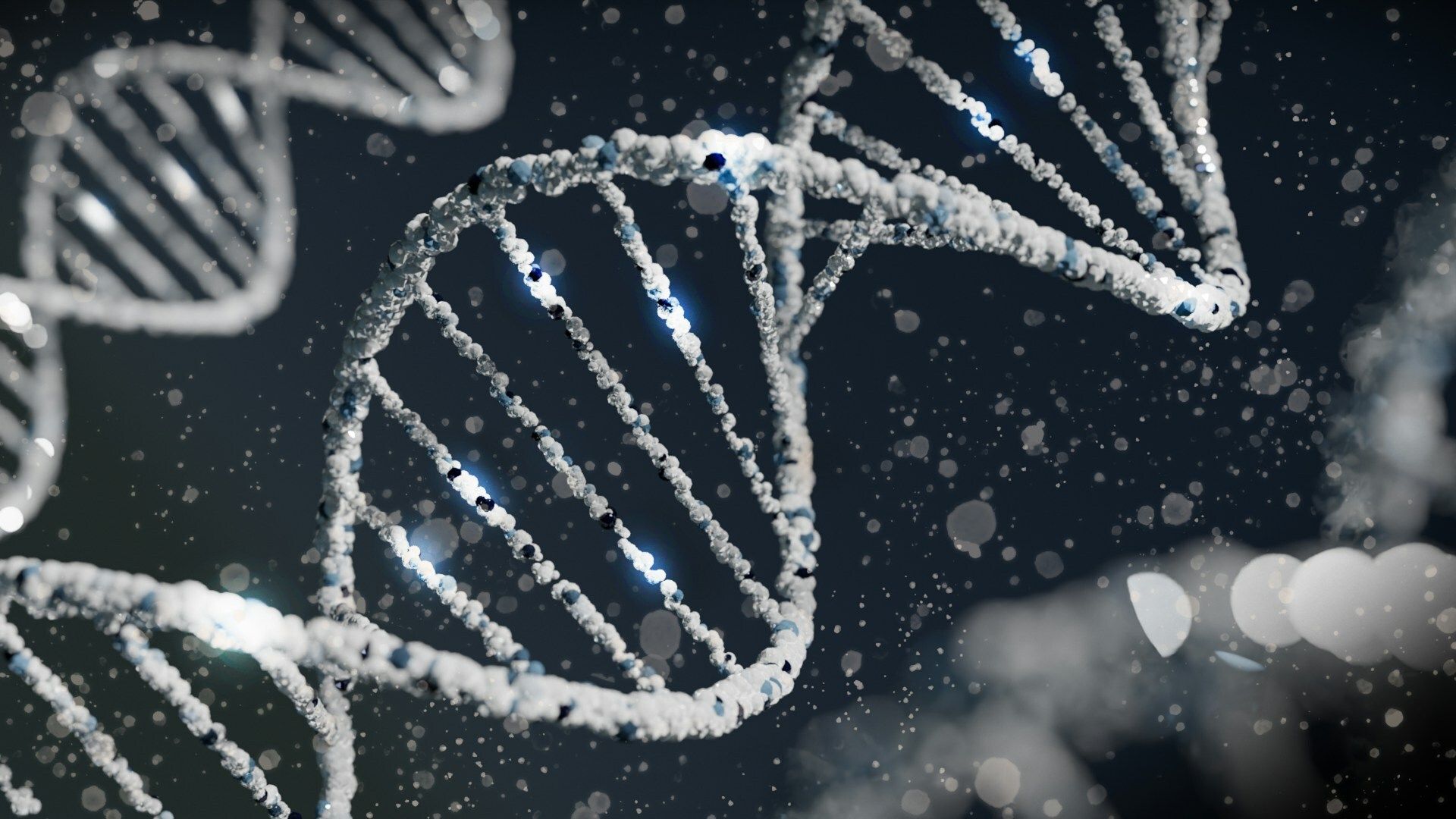
In 2025, gene editing moved from experimental promise to tangible clinical impact. A one time CRISPR Cas9 based therapy produced deep and durable suppression of transthyretin in patients with hereditary transthyretin amyloidosis with polyneuropathy, a progressive and often fatal multisystem disease.
In an early phase study, a single infusion of nexiguran ziclumeran reduced circulating transthyretin levels by approximately 90 percent within weeks, with suppression sustained through 24 months. Most patients demonstrated stabilization or improvement in polyneuropathy stage and disability scores, a meaningful outcome in a disease typically marked by steady progression.
Unlike existing therapies that require lifelong dosing to silence TTR production, this approach permanently inactivates the TTR gene in the liver using in vivo CRISPR Cas9 delivered via lipid nanoparticles. Adverse events were largely transient, and the safety profile supported continued development.
While longer follow up and larger trials are needed, this study marks a pivotal moment. In 2025, gene editing became a credible therapeutic strategy in humans, signaling a shift toward one time, disease modifying treatments for inherited disorders.
Source: NEJM
MASLD Redefines Fatty Liver Disease
Why metabolic risk, not steatosis alone, defines prognosis in 2025
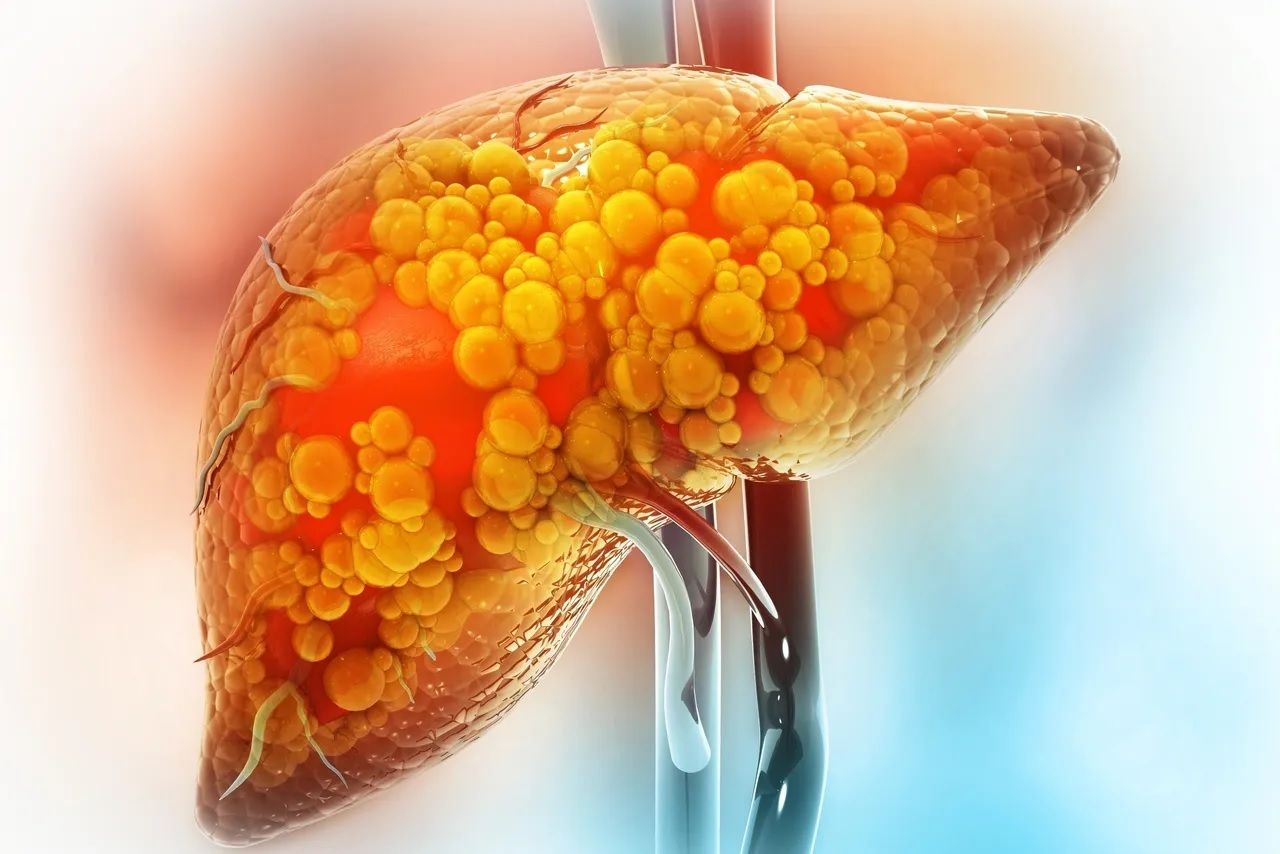
Although the term MASLD was introduced in 2023, 2025 is the year it became clinically decisive. Large population analyses and meta analyses now show that outcomes in metabolic dysfunction–associated steatotic liver disease are driven primarily by cardiometabolic risk burden, not by liver fat in isolation.
Data from national cohorts demonstrate that adults with MASLD and multiple metabolic risk factors such as diabetes, hypertension, and dyslipidemia face substantially higher all cause and cardiovascular mortality compared with those with isolated steatosis. Cardiovascular disease, not liver failure, remains the leading cause of death across MASLD populations, even when fibrosis stage is similar. This confirms MASLD as a systemic metabolic disorder with hepatic manifestations rather than a liver limited condition.
Comparative analyses further clarify that MASLD carries a distinct risk profile compared with alcohol associated or mixed etiology steatotic liver disease. While fibrosis severity remains prognostically important, metabolic context meaningfully modifies outcomes at every stage of disease. As a result, liver enzymes alone are no longer adequate for risk stratification.
The implication for practice in 2025 is clear. MASLD reframes fatty liver disease around who is at highest cardiometabolic risk and who benefits from early intervention, not simply who has steatosis on imaging. Using MASLD in Clinical Chronicle reflects this shift. It aligns language with outcomes, reinforces upstream prevention, and anchors hepatology firmly within the broader framework of cardiometabolic medicine.
Source: THELANCET
Endocrinology’s Next Leap Beyond GLP-1
Triple-agonist therapy pushes medical weight loss into surgical territory
In 2025, obesity treatment crossed a new threshold as Eli Lilly’s triple-agonist Retatrutide delivered the greatest weight loss yet reported in a late-stage pharmacologic trial, along with meaningful improvements in obesity-related joint disease. Medical therapy began to rival bariatric surgery not only in magnitude of weight loss, but in functional benefit.
In the TRIUMPH-4 trial, patients receiving the highest dose lost nearly one quarter of their body weight at 68 weeks, with even greater reductions among those who remained on therapy. This weight loss translated into clinically important outcomes. Knee osteoarthritis pain fell by more than 60 percent on average, and some patients became pain-free, reinforcing obesity treatment as therapy for disabling disease rather than risk reduction alone.
Retatrutide’s potency reflects its triple-agonist mechanism, targeting GLP-1, GIP, and glucagon receptors simultaneously. This increased efficacy came with higher gastrointestinal side effects and discontinuation rates, particularly in patients with lower baseline BMI, suggesting its greatest role may be in severe obesity.
The implication is clear. In 2025, endocrinology moved beyond incremental GLP-1 advances into an era of high-intensity, disease-modifying obesity pharmacotherapy, with outcomes once achievable only through surgery.
Source: LILLY
Cardiology
Cardioprotection: GLP-1 and SGLT2 Is Not One Size Fits All
Cardiovascular Benefit Diverges by Age, Even as HbA1c Moves in Opposite Directions

UNSPLASH
In 2025, diabetes care moved beyond glucose centric thinking. A large network meta analysis showed that cardiovascular protection from SGLT2 inhibitors and GLP 1 receptor agonists varies meaningfully by age, even when HbA1c reduction does not.
Across more than 600 trials, SGLT2 inhibitors delivered greater cardiovascular benefit with increasing age. For every 30 year increase in age, SGLT2 inhibitors were associated with a 24 percent greater relative reduction in major adverse cardiovascular events, despite diminishing glycemic effect. HbA1c lowering fell by about 0.2 percent per 30 years of age, underscoring that cardioprotection occurred independently of glucose control.
In contrast, GLP 1 receptor agonists showed the opposite pattern. Cardiovascular benefit declined with age, with a higher relative risk of MACE per 30 year age increase, while HbA1c reduction improved in older adults when used as mono or dual therapy. Sex did not modify outcomes for either drug class.
The clinical message was clear. HbA1c is an incomplete surrogate for cardiovascular risk. In older adults with type 2 diabetes, SGLT2 inhibitors may offer disproportionate heart protection even when glucose lowering is modest, while younger patients may derive greater cardiovascular benefit from GLP 1 based therapy. Age, not sex, emerged as a key determinant of therapeutic value.
Source: JAMA
TAVR Moves Earlier and Proves It Can Last
Why 2025 Changed the Aortic Stenosis Paradigm
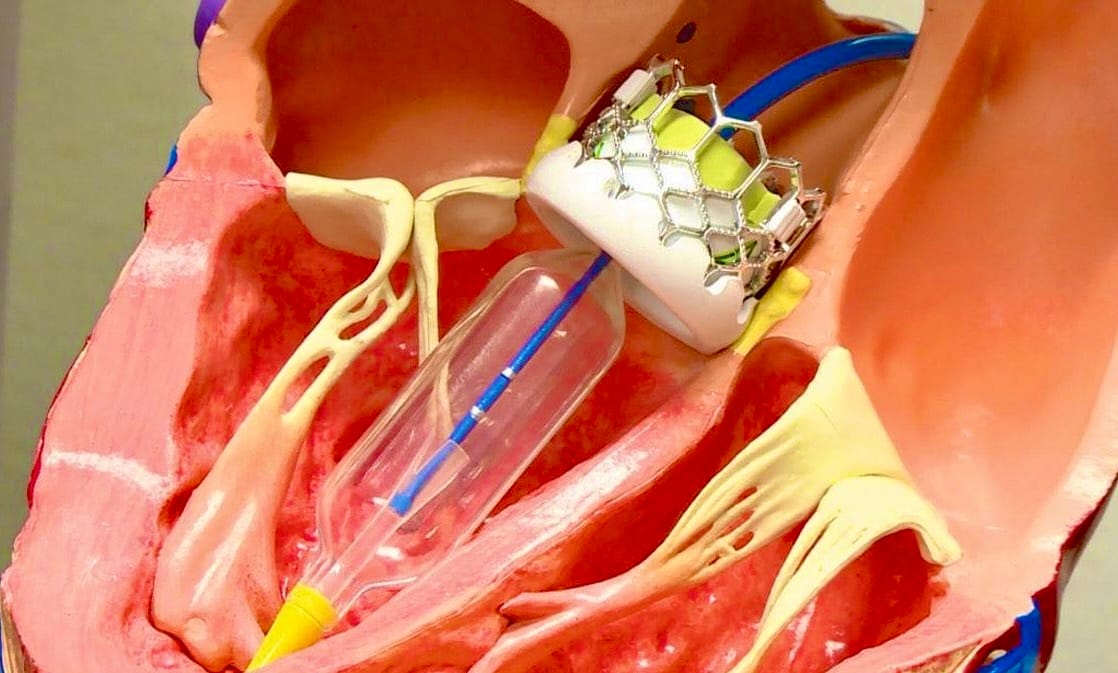
In 2025, transcatheter aortic valve replacement crossed two long standing thresholds. Evidence supported intervening before symptoms develop, and long term data reassured clinicians that durability in low risk patients approaches surgical replacement.
The EARLY TAVR trial showed that preemptive TAVR in asymptomatic severe aortic stenosis reduced the composite of death, stroke, or unplanned cardiovascular hospitalization compared with clinical surveillance. Over a median 3.8 years, events occurred in 26.8% of patients treated upfront versus 45.3% with watchful waiting, driven largely by fewer unplanned hospitalizations. Nearly 87% of patients in the surveillance arm ultimately required valve replacement, underscoring that delay often meant deferral rather than avoidance.
At the same time, seven year data from the PARTNER 3 trial addressed durability concerns in low risk patients. The composite of death, stroke, or rehospitalization was similar between TAVR and surgical valve replacement at 7 years, with excellent and sustained valve hemodynamics in both groups. Rates of reintervention were low and comparable, while new onset atrial fibrillation remained substantially lower with TAVR.
Together, these trials reframed aortic stenosis management. TAVR is no longer just an option for symptomatic disease or short term benefit. In carefully selected patients, it can be performed earlier to prevent clinical deterioration and with growing confidence in long term performance, shifting the paradigm from reactive replacement to proactive intervention.
Source: NEJM
Lenacapavir Advances Twice-Yearly HIV Prevention With CDC Support
FDA Cleared, CDC Backed
In 2025, long-acting HIV prevention crossed from breakthrough to standard of care. After FDA approval earlier in the year, the CDC issued a strong recommendation for twice-yearly injectable lenacapavir for HIV pre-exposure prophylaxis, cementing its role in routine prevention strategies.
The CDC endorsed lenacapavir as a highly effective and safe PrEP option administered every 6 months, citing high-certainty evidence from phase III PURPOSE 1 and PURPOSE 2 trials. Lenacapavir showed 100% efficacy in adolescent girls and young women in Africa and reduced HIV incidence by 96% versus no PrEP and 89% versus daily oral PrEP in cisgender men and transgender or gender-nonbinary persons. Adverse events were comparable to oral PrEP, with injection-site reactions most common, and use was supported in pregnancy when HIV risk remains high.
What distinguishes 2025 is not the efficacy alone but the endorsement. CDC backing places lenacapavir alongside oral PrEP and cabotegravir in national guidance, directly addressing adherence and stigma barriers associated with daily dosing. However, real-world access remains uneven. At roughly $28,000 per year, insurance coverage varies across payers, with some Medicaid programs and PBMs covering the drug while others have declined, making guideline support critical for broader uptake.
Clinical Takeaway
Lenacapavir’s twice-yearly dosing, near-complete prevention efficacy, and CDC endorsement mark the most significant advance in HIV prevention in years. The remaining challenge is not clinical effectiveness, but ensuring equitable access so this paradigm-shifting option reaches the populations that need it most.
Source: NEJM
SGLT2 Inhibitors Expand Across the Full Spectrum of CKD
No Longer Limited by Diabetes or Albuminuria
In 2025, meta-analyses provided the strongest evidence to date that SGLT2 inhibitors slow chronic kidney disease progression across a far broader population than previously targeted, challenging albuminuria and diabetes based treatment restrictions.
Across more than 70,000 patients from 10 randomized trials, SGLT2 inhibitors reduced the risk of CKD progression at every level of baseline kidney function, including stage 4 disease. Hazard ratios ranged from 0.57 to 0.71 across eGFR strata, confirming that lower eGFR should not preclude initiation.
Kidney protection was also independent of albuminuria and diabetes status. Patients with minimal, moderate, or severe albuminuria all derived benefit, as did patients with and without diabetes, with hazard ratios of 0.65 and 0.74 respectively.
Adverse events were uncommon. SGLT2 inhibitors reduced risks of acute kidney injury and hospitalization, with increased ketoacidosis risk limited to patients with diabetes. The clinical message was clear: SGLT2 inhibitors should be considered foundational therapy across the CKD spectrum, with underutilization now the primary gap in care.
Source: JAMA
Biologics Finally Gain a Foothold in COPD
Targeted Biologics Begin to Reshape COPD Care

For years, biologics in COPD produced more disappointment than progress. In 2025, that narrative shifted. While inhaled triple therapy reached its ceiling, biologics targeting type 2 inflammation began delivering reproducible benefits in carefully selected patients, marking the first credible step toward personalized COPD treatment.
Dupilumab became the first biologic to break through, earning FDA approval after the BOREAS and NOTUS trials showed significant exacerbation reduction in patients with frequent exacerbations, chronic bronchitis, and blood eosinophil counts ≥300 cells/μL. These trials demonstrated not only fewer exacerbations but modest improvements in lung function and health status, establishing proof that biologic modulation can work in the right COPD phenotype.
Momentum continued with the phase III MATINEE trial, where mepolizumab reduced moderate or severe exacerbations by 29% when added to triple inhaled therapy in eosinophilic COPD. Time to first exacerbation was significantly prolonged, and safety was reassuring, though effects on lung function and quality of life were limited. These findings reinforced that IL-5 pathway inhibition may benefit a subset of patients, even if not yet ready for broad clinical adoption.
Clinical Takeaway
Biologics are no longer theoretical in COPD. The 2025 evidence supports a phenotype-driven approach, particularly for eosinophilic frequent exacerbators who remain uncontrolled on maximal inhaled therapy. Biologics are not for everyone, but for the right patient, they represent the first meaningful expansion of COPD treatment in over a decade, with guidelines evolving cautiously alongside the evidence.
Source: NEJM
Small Cell Lung Cancer Finally Moves Forward
Maintenance Survival Gains and Immune Engagement Mark a Turning Point

In 2025, small cell lung cancer experienced its most meaningful progress in decades, with advances that improved survival in both frontline maintenance and relapsed disease, breaking a long period of therapeutic stagnation.
The most immediate practice-changing advance was the FDA approval of lurbinectedin plus atezolizumab as first-line maintenance therapy for extensive-stage disease. In the phase III IMforte trial, adding lurbinectedin to maintenance atezolizumab more than doubled progression-free survival from 2.1 to 5.4 months and improved overall survival from 10.6 to 13.2 months. This approval transformed the post-induction phase from passive observation to active disease control for patients without progression after carboplatin, etoposide, and atezolizumab.
At the same time, progress emerged in the relapsed setting with tarlatamab, a DLL3-targeted bispecific T-cell engager, which demonstrated meaningful overall survival improvement in previously treated extensive-stage small cell lung cancer and received regulatory approval. Alongside early signals from emerging antibody–drug conjugates, this marked the first real success of immune-engaging strategies in a disease long resistant to innovation.
Clinical Takeaway
For the first time in years, small cell lung cancer advanced on multiple fronts. Maintenance therapy now delivers a proven survival benefit in frontline care, while novel immune-based therapies offer new hope after relapse. Together, these developments made 2025 the most consequential year for small cell lung cancer in a generation.
Source: FDA
Over time, medicine teaches us that clarity doesn’t come from knowing more, but from listening better and acting with intention for the patient in front of us.
Until next time,

Be relentless. Save lives.

